Uterine fibroid
What is a fibroid?
A uterine fibroid is also called a myoma of leiomyoma. It is a benign growth of muscle cells in the muscle layer of the uterus. A uterine fibroid can be on the outside of the uterus, in the uterine wall itself or in the uterine cavity. How a uterine fibroid is formed is not entirely known. A uterine fibroid can be a few millimeters, but also more than 10 centimeters.
A uterine fibroid occurs in about 70 percent of women, but causes complaints in about 25 percent. It is thought that growth occurs under the influence of female hormones. That is why a uterine fibroid never grows before the first menstruation. After menopause, uterine fibroids usually become smaller and the complaints less.
More often, uterine fibroids develop in women who do not (yet) have children and in women of African descent. A uterine fibroid usually does not cause any problems when becoming pregnant or during pregnancy, but can sometimes grow due to hormonal changes during pregnancy. After pregnancy, the uterine fibroids often become smaller again.
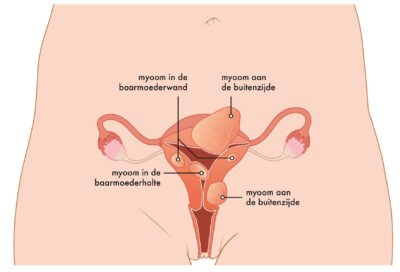
Example of multiple uterine fibroids (isala.nl)
Symptoms
What symptoms does a fibroid cause?
A uterine fibroid usually gives little or no symptoms and is often found by accident. Most uterine fibroids grow slowly and go unnoticed. The location of the uterine fibroid has more influence on the complaints than the size. For example, fibroids in the uterine cavity, even if small, can cause menstrual complaints. The most common complaints are excessive blood loss and menstrual pain. In principle, menstrual periods remain regular. The extensive loss of blood, possibly with clots, can cause anemia, which can make a woman, feel tired or short of breath.
Other, rarer complaints of uterine fibroids are an oppressive feeling in the abdomen, pain low in the back, complaints with urination and complaints of pain and/or blood loss during sex. Very rarely a uterine fibroid shrivels due to a lack of blood supply, resulting in severe abdominal pain. The chance that uterine fibroids become malignant is very small. This occurs in 1 in 400 to 4000 women.
Diagnosis
How are fibroids diagnosed?
When a uterine fibroid is suspected, the normal gynecological examination takes place. The gynecologist looks at the cervix with the help of a spreader (speculum). The gynecologist also feels the uterus and ovaries. He/she does this by inserting one or two fingers into the vagina and feeling the abdomen with the other hand. This is called a vaginal toucher. The gynecologist then uses an internal ultrasound to assess the location and size of the uterine fibroid. The gynecologist inserts a thin ultrasound head into the vagina and examines the uterus and ovaries.
If there is a lot of blood loss or fatigue, the doctor can check the iron level of the blood (Hb or hemoglobin) to see if there is anemia.
For additional assessment of uterine fibroids, there are other examinations, such as contrast ultrasound, hysteroscopy or an MRI scan. Usually only an ultrasound scan is sufficient.
In a water contrast-ultrasound (also called a SIS-ultrasound: Saline Infusion Sonohysterography) the gynecologist places a spreader to insert a thin tube into the uterus. The gynecologist then injects a small amount of water or gel into the uterus and makes another internal ultrasound. In this way, the gynecologist can see the uterine cavity and the fibroid better. This examination often gives some abdominal cramps.
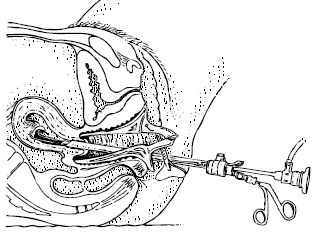
Hysteroscopy literally means looking into the uterus. The gynecologist inserts a thin tube with a camera into the vagina and slides it into the uterus. This can be painful, because the uterus reacts to it. Through this tube, the gynecologist brings water into the uterus so it expands a little. Now the gynecologist can see the inside of the uterus. The gynecologist can see if there is a fibroid in the uterus or protrudes into the uterine cavity.
The gynecologist has an MRI scan made if an internal ultrasound is not sufficient to assess the size and location of the uterine fibroid. The gynecologist can also have an MRI-scan made if he/she is in doubt whether it is a uterine fibroid.
Treatments
What treatments are possible for a fibroid?
If you have no complaints, nothing needs to be done about uterine fibroids and no further control is necessary. If there are complaints, the woman chooses a treatment together with the gynecologist. The type of symptoms, the number , the location and size of the fibroids, your age, any desire to become pregnant and your preference for the type of treatment will all be taken into account. You can choose from several treatment options:
Medication
There is medical treatment with and without hormones. Medicines try to reduce the amount of blood loss and/or menstrual pain. The uterine fibroids remain; sometimes they get a little smaller. The effect of the medication depends on the amount, size and location of the uterine fibroid. After stopping the medication, the symptoms usually return.
isala.nl
Hysteroscopy
In this procedure, the gynecologist removes a fibroid located in the uterus or bulging in the uterine cavity through the vagina. He or she will use a viewing tube. For this operation, you will be under anesthesia or receive an epidural.
Embolization
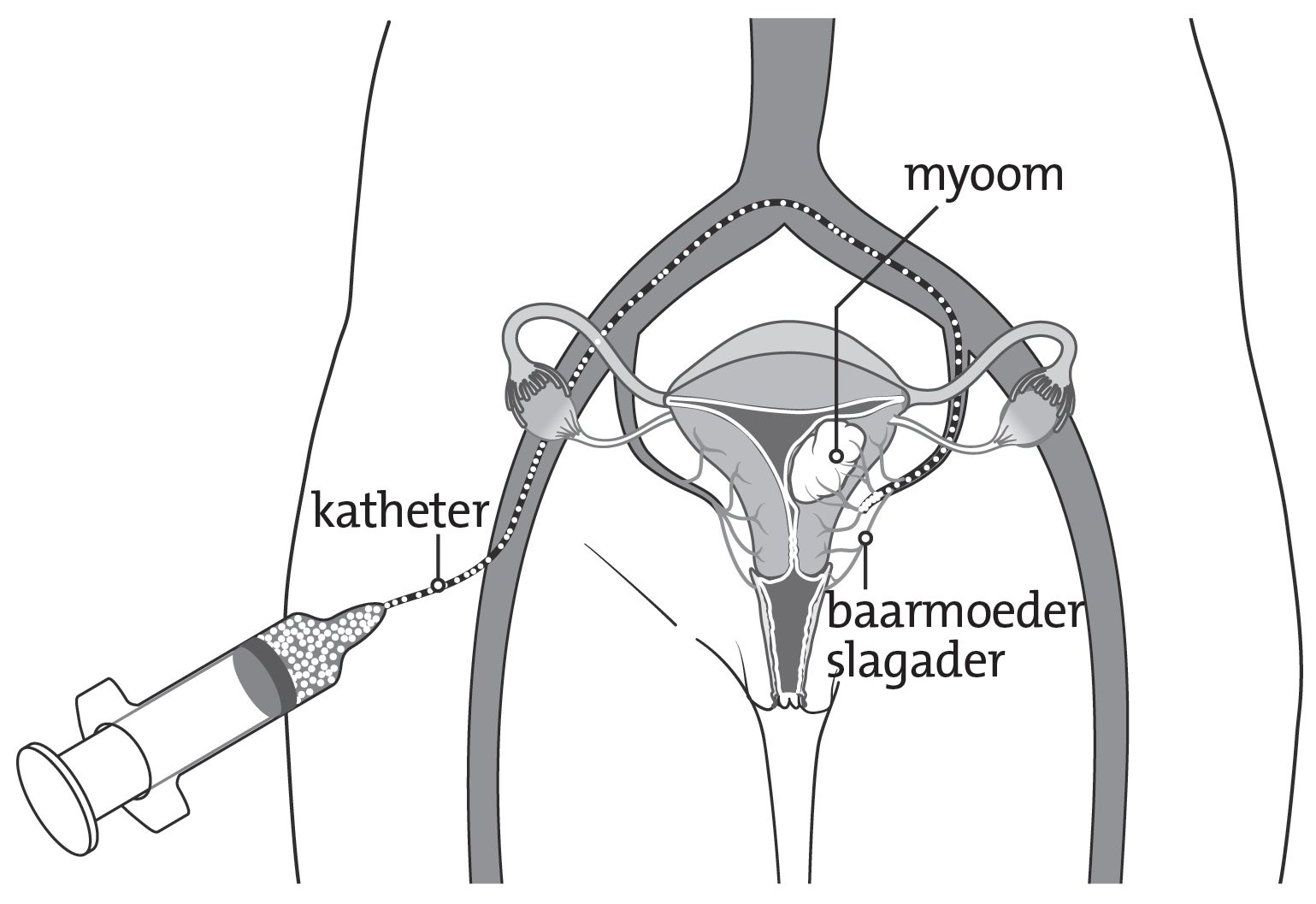
isala.nl
During an embolization treatment, blood vessels leading to the fibroid are closed by filling them with small particles. These blood vessels are reached by moving a catheter via a vein of the groin all the way up to the uterine fibroids, which is all visualized by real-time angiography. Because the uterine fibroids now no longer receive blood, cell dead of the fibroid tissue will take place. Embolization is performed in the X-ray department by a radiologist.
Surgical removal of the fibroid (myomectomy)
If the fibroid is on the outside of the uterus or in the wall of the uterus, the gynecologist can surgically peel out the fibroid. This is called a surgical removal of a fibroid or myomectomy. A surgical removal of a fibroid can be done through laparoscopy or laparotomy. This treatment preserves the uterus itself. However, after fibroid surgery, adhesions may form in the cavity of the uterus, which may make it difficult to conceive. If the uterus is opened during the surgical removal of the fibroid, the gynecologist will recommend a C-section for future pregnancy.
Surgical removal of the uterus (hysterectomy)
Sometimes complete removal of the uterus is the best solution for the complaints. This is called surgical removal of the uterus or hysterectomy. This eliminates the blood loss; the effect on abdominal or back pain is less predictable. The uterus can sometimes be removed through the vagina, but in fibroids, this is usually done through the abdomen. This can be performed by means of laparoscopy or laparotomy. In principle, the ovaries and fallopian tubes remain in the abdomen. Fibroids cannot grow back after the uterus has been removed. Therefore, the surgical removal of the uterus is seen as the most definitive treatment.
MR-HIFU
MR-HIFU (Magnetic Resonance guided High Intensity Focused Ultrasound, a combination of MRI and ultrasound) is a relatively new treatment for women with uterine fibroids. The treatment started in 2009 at the University Medical Center Utrecht and at Isala women have been treated since 2016. Several thousand women worldwide have now undergone the treatment. This treatment is performed by the radiologist and takes place in day treatment. You do not need to stay overnight in the hospital after this treatment. More information can be found on the MR-HIFU page.
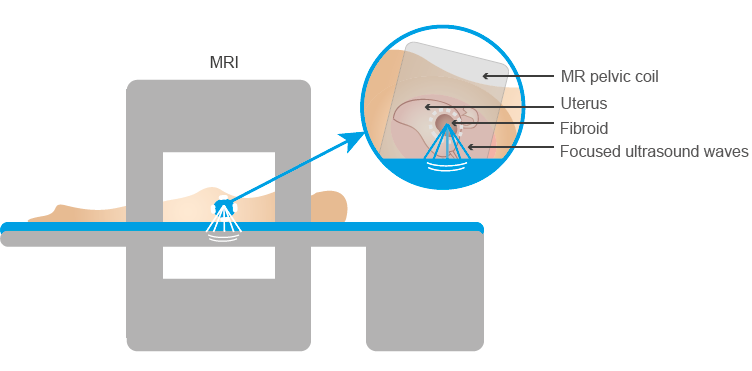
Position in MRI during MR-HIFU treatment for uterine fibroids (profoundmedical.com/sonalleve/)
To finalize
To finalize
Uterine fibroids can cause symptoms, but they are not life threatening. Usually there is enough time to think about the different treatments and make a decision. The gynecologist can give you the best advice.
The texts above are based on the information available through DeGynaecoloog. DeGynaecoloog is an initiative of the Dutch Society for Obstetrics and Gynecology (NVOG). With this website, they provide reliable information and want to offer support in making decisions when it comes to health. Healthcare providers in collaboration with patients or patient associations have developed all the information that can be found on that website.
Links
Links
https://www.degynaecoloog.nl/onderwerpen/vleesboom/#wat-is-een-vleesboom
https://www.isala.nl/patientenfolders/5375-myomen/
https://www.isala.nl/patientenfolders/6113-behandeling-van-een-vleesboom-myoomembolisatie/
https://www.isala.nl/patientenfolders/7626-mr-hifu-bij-vleesbomen/
Frequently asked questions
Frequently asked questions
1. I am diagnosed with a uterine fibroid, should I have it treated?
Treatment of a uterine fibroid is not always necessary. Many women have uterine fibroids without symptoms. If you have any complaints as a result of your uterine fibroid, it is wise to contact your family doctor or gynecologist.
2. Can I become pregnant with a uterine fibroid?
Usually a uterine fibroid does not cause any problems when you get pregnant or during your pregnancy. Sometimes it is possible that there are so many (large) fibroids present in the wall of your uterus or in the uterine cavity, that it causes problems with implanting of an embryo or growing a baby. This is different for each woman. During pregnancy, it is possible that the uterine fibroid grows and causes pain. Sometimes women cannot give birth vaginally because of the location of the uterine fibroid. They have to give birth through a caesarean section. For more information about your specific situation, it is best to contact your gynecologist.
3. Can I become pregnant after a fibroid treatment?
If you would like to be treated for your fibroid, it is always important to consider if you would like to become pregnant in the future. The most effective treatment for fibroids is uterine surgery (hysterectomy). This removes the entire uterus but makes pregnancy impossible. There are alternatives to uterine surgery, but which treatment is most appropriate depends on your situation. After a fibroid surgery, embolization or MR-HIFU treatment, you may become pregnant in most cases. However, you are advised to stay under the control of your gynecologist during pregnancy and you may be advised to give birth by caesarean section. For more information about your specific situation, it is best to contact your gynecologist.
4. I am not allowed/willing to take medical treatment, but I can’t have my uterus removed, can I be treated in any other way?
In the past, the only treatment for uterine fibroids, if medication did not help or was not possible, was surgical removal of the uterus (hysterectomy). This is a major operation with often a long recovery time. That is why less invasive treatments have been developed in recent years, including MR-HIFU treatment and embolization. Not all women are eligible for these treatments. Moreover, the big disadvantage of both treatments is that the symptoms of the fibroids can return after a few years with regrowth or new growth of fibroids. More information about the treatments themselves can be found above.
5. Is a uterine fibroid a form of cancer?
Uterine fibroids are also called benign tumors or tumors. This can be confusing because it sounds like a form of cancer, but it is not. Although the fibroids grow, this happens in a different way than with cancer of the uterus. Sometimes it is difficult to tell from an ultrasound or MRI scan whether a swelling is benign (fibroids) or malignant (cancers). In about 1 in 400 to 4000 women, such a swelling turns out to be cancer. If you have specific questions about this, it is best to contact your gynecologist.